Berry beneficial: Blueberry consumption alleviates abdominal pain in gastrointestinal disorders
In a recent study published in the journal Nutrients, researchers investigate whether blueberry consumption could improve the clinical outcomes, functioning, and overall quality of life of individuals with functional gastrointestinal disorders (FGID).

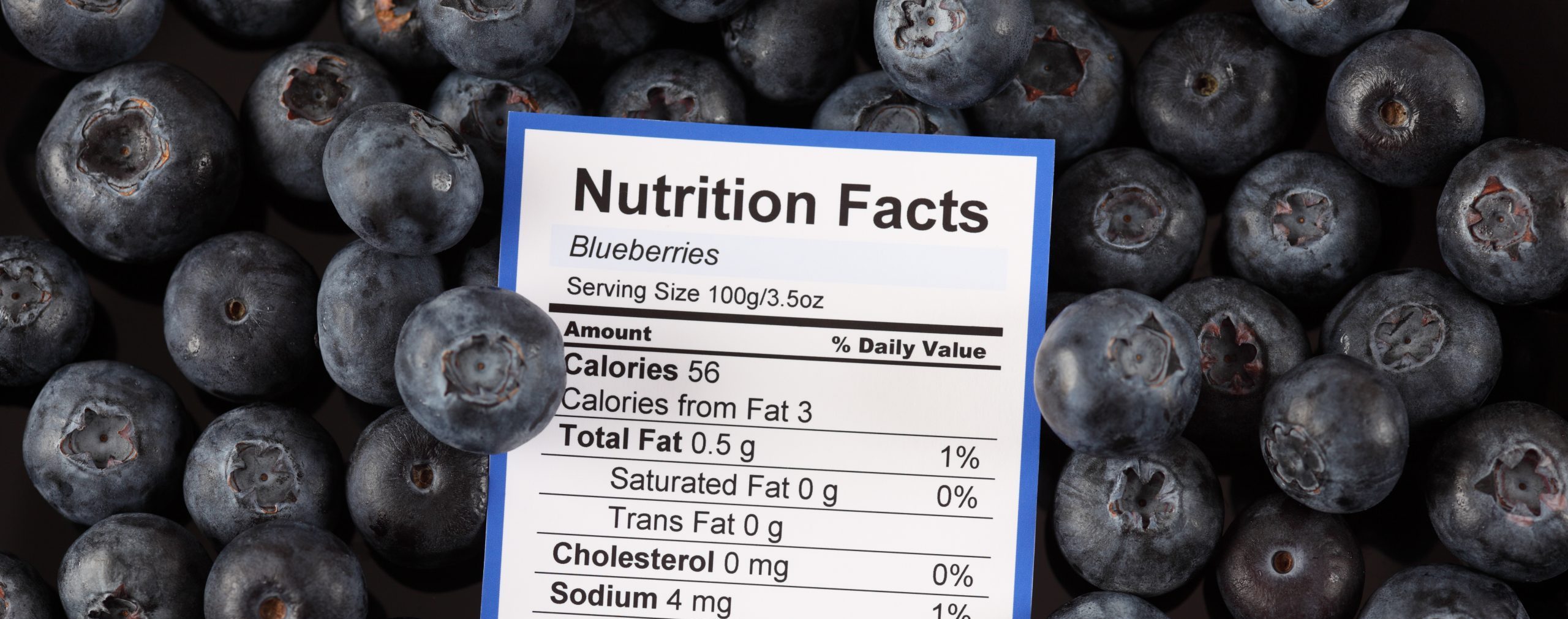
Study: Blueberries Improve Abdominal Symptoms, WellBeing and Functioning in Patients with Functional Gastrointestinal Disorders. Image Credit: Bukhta Yurii / Shutterstock.com
Background
FGID impact 10-15% of most populations and often involves functional dyspepsia and irritable bowel syndrome (IBS). While the specific mechanisms of FGID remain unclear, certain factors, such as sensitization of the nervous system, gut permeability modulation, immune activation, and enteric microbiome changes, are thought to be interrelated and impacted by dietary factors.
Enteric microbiota are believed to play a vital role in many of the mechanisms of FGID. Furthermore, dietary components can influence enteric microbiota with downstream epigenetic changes in the host.
One of the most common antioxidants in food is polyphenols, which are the most abundant metabolites found in plants. Blueberries are rich in polyphenols, with various epidemiological and mechanistic studies reporting that regular consumption of blueberries is linked to a reduced risk of type 2 diabetes and cardiovascular diseases, as well as improvements in visual and brain function.
However, despite the anti-inflammatory, antioxidant, neuroprotective, and membrane permeability reversing properties of blueberries that could benefit FGID patients, there remains a lack of clinical studies involving FGID patients that examined the impact of blueberry consumption.
About the study
In the present study, researchers examine the impact of blueberry consumption on the laboratory measures and clinical symptoms of FGID. These results were compared to those of a placebo with matching sugar composition but no polyphenol or dietary fiber content.
FGID patients were enrolled in a double-blind, randomized, placebo-controlled cross-over, two-arm, single-center study. White male or female patients between the ages of 18 and 60 years within a specific body mass index (BMI) range, having IBS or functional dyspepsia, were enrolled in the study.
Participants were excluded if there was evidence of other diseases that were clinically significant in the medical history, stool or blood tests, endoscopy, ultrasound, or computerized tomography (CT) scan. Individuals who began taking new medications during the study period had probiotics or antibiotics two weeks preceding the study or during the study, were pregnant or breastfeeding, had a colonoscopy, or had planned dietary modifications were excluded.
Various questionnaires were used to determine baseline demographic data, gastrointestinal, extra-gastrointestinal, depression, and anxiety symptoms and assess dietary habits and personal history. The Bristol stool scale was used to determine stool consistency. Furthermore, fructose breath tests were used to measure methane and hydrogen concentrations in breath, along with the occurrence of symptoms such as heartburn, abdominal pain, diarrhea, flatulence, borborygmi, and nausea.
The treatment consisted of freeze-dried blueberry powder with measured nutritional composition, while the control consisted of taste-matched blueberry powder placebo with matching sugar composition without the polyphenol and fiber content. Both treatment and placebo were taken twice a day in 15 g doses after meals.
Blueberries improve quality of life and abdominal pain in FGID patients
About 53% of patients reported relief in abdominal pain symptoms after blueberry treatment as compared to placebo at 30%. Although the total Gastrointestinal Clinical Rating Scale and pain scores were not significantly different between the blueberry treatment and placebo groups, the ratings for life functioning and quality of life improved after blueberry treatment as compared to the placebo.
Six weeks of blueberry treatment resulted in significant improvement in abdominal pain symptoms, which was one of the two primary outcomes examined. Secondary outcomes, including life functioning, quality of life, and overall well-being, were also improved as compared to the placebo. These quality-of-life improvements may be partly influenced by the alleviation of gastrointestinal symptoms.
For the other measures, the differences in treatment effects were not statistically significant. However, the relief in abdominal pain and overall improvements in life function and quality of life scores after blueberry treatment as compared to placebo indicated that the dietary fiber and polyphenol composition of blueberries, rather than the sugar content, was responsible for the beneficial effects.
Conclusions
The polyphenol and dietary fiber content of blueberries can significantly reduce abdominal pain and improve the quality of life in FGID patients. While the other markers of gastrointestinal function did not significantly differ between the blueberry treatment and placebo groups, the results suggest that the broad benefits exerted by the blueberry diet were not related to the sugar content of blueberries.
24/05/2023